Author: Mark Kelly, Ad Dip Myo, Registered Myotherapist
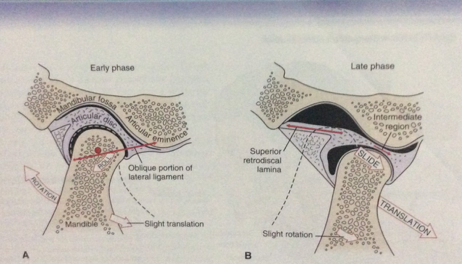
Temporomandibular joint pain and dysfunction (TMJPD) effects people of all ages, the condition present with either acute or chronic pain in the joint between the Jaw bone (Mandible) and the skull (Temporal Bone). Normal function at this joint allows us to chew, speak, and swallow where right and left sides have to move in a coordinated fashion. Movements occurring here are due to the unique shape of the joint surfaces and from a number of specific pares of muscles acting on the joint, that either open or close the mouth. There is a cartilage disc that is located within the joint. The joint is enclosed by a capsule that contains synovial fluid this fluid lubricates the joint. In normal opening and closing the disc enables more space to be available between the joint’s surfaces allowing for effective movement. When opening the mouth, the jaw rotates downward at the same time as it translates forward this enables a greater bite (S Krohn, 2020). As the mouth opens a muscle that attaches to the front of the joint called the Lateral Pterygoid pulls the jaw bone and the disc in a forward and slightly downward direction to various degrees depending on how much opening is needed. A series of small ligaments (lateral temporomandibular, sphenimandibular and Stylo mandibular) assist in guiding movement and position of the joint and disc. When closing the mouth, the jaw performs the reverse action (D Magee 2008). With TMJPD what can occur is the disc that separates the joint surfaces may become displaced resulting in pain, clicking or clunking upon movement.
( Magee 2008)
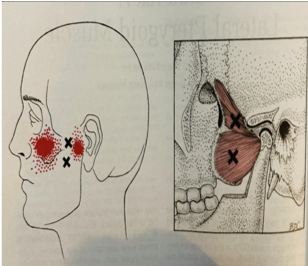
( Simons & Travell, 1999)
The problem:
There are generally two types termed disc displacement without reduction (disc sits in a forward and inward orientation). In this type problems with TMJ function are more significant and painful locking can occur reducing the ability to open the mouth and even lock jaw movement which may require more extensive treatment depending on severity) the other type is disc displacement with reduction on jaw movement there can be some pain or clicking or joint sounds when eating but the disc tends to go back into where it should normally be (G Klasser 2020). The TMJ disc is largely avascular (without blood) and anural (without nerve tissue in areas where the disc takes load however the outer parts of the disc and joint capsule that encases the joint and disc does have nerve and vascular structures which tend to be more pain producing when the is a problem and if there is inflammation (Magee, 2008)
Contributing factors to dysfunction and pain:
Muscle imbalance is a major factor leading to TMJ dysfunction. Changes in muscle recruitment patterns increases stress on the joint surfaces causing local pain, headaches or even toothache type pain can be due to referred pain from fatigued muscles with trigger points (Simons & Travell, 1999). There can be potential damage to the joint resulting in acute or chronic inflammation. Intrinsic Factors that can affect the function of the jaw include poor posture, people who experience high levels of stress or anxiety, and also those who clench or grind the teeth. Extrinsic factors include trauma such as a blow to the jaw.
Other conditions that can predispose TMJ dysfunction include Rheumatoid Arthritis which is an autoimmune disease involving multiple joints. Various aspects of mental health such as anxiety and high stress levels which contribute to bruxism (griding) or clenching the teeth (especially chronic in nature), (NIH, 2017). Other conditions such Chronic Fatigue Syndrome (a condition that manifests with severe levels of fatigue and sleep disturbances) and Fibromyalgia (a condition that is associated with malty region increased pain perception and stiffness in which fatigue and sleep disturbances are also noticed. Other factors may include bone diseases or metastasis, respiratory tract or sinus infections.
Increased states of anxiety or stress and depression have been shown to be contributing factors to TMJP (L Bonjardim, 2005).
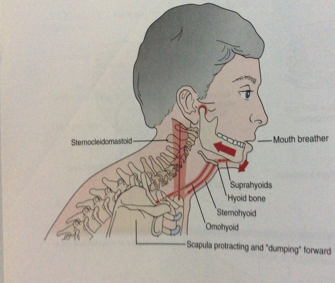
In Mouth breathers the position of the tongue changes slightly and encourages increased use of extra inspiratory muscles (muscles located in the neck and ribs) used when in need of increased breathing. Resulting in these muscles becoming fatigued and tight.
Assessment:
Assessment is performed by the clinician to establish factors associated with initial onset and signs and symptoms such as radiating jaw and or face pain with restricted movement, how long they have been present for and the how severe the patient s problem is. The clinician will gain information about whether pain is associated with closing which can assist in determining whether there is a problem inside the joint capsule (intracapsular) such as, disc displacement or arthritis. If there is more pain associated with opening this can assist in determining problems outside of the joint capsule such as muscle, ligament or connective tissue involvement (D Magee 2006). A previous history of Dental related problems can change chewing mechanics to overuse or compensate with one side more dominantly, this change initially can go unnoticed as its somewhat natural for the body to do this. Over time however this altered mechanical pattern can create occlusion changes (changes in the way the teeth specifically the molar’s contact each other). Muscles start to become fatigued, strained and contribute to instability and deceased coordination (S Prater, 2012). The clinician will also gain information about the 24-hour pain pattern e.g., morning Pain from Arthritis or fatigue strain in muscles associated with night clenching or bruxism.
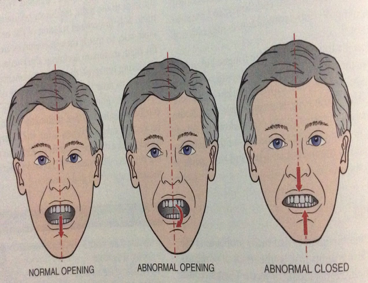
(Magee, 2008)
(Magee, 2008)
Clinical observations:
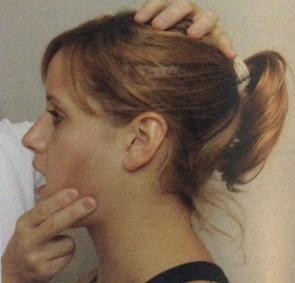
Once obtaining a history the clinician will aim to get some objective information via feeling the tissue of the MTJ and associated muscles. The clinician will also observe posture alignment and range of movement of the face and jaw, as well as performing the same for other regions of the neck, shoulders and back as these factors are important to include as they can contribute to increased forward head position. There is evidence that indicates a change of the length tension relationship between the supra and infra hyoid muscles (muscles located bellow the jaw attaching to the hyoid bone) and other muscles located toward the region just behind the TMJ and upper part of the back of the neck. Imbalances between these muscle groups can contribute to decreased range of motion on either side of the jaw. Additionally, with a forward head position this changes the of angle of the jaw encouraging the mandible bone to sit in a more backward and upward position increasing the potential for the joint to become compressed (M Mulet, 2007).
(Magee 2008)
Management:
In majority of cases conservative treatment is effective and recommended prior to more invasive investigation and treatments such as surgery (R, Poluha 2019). During more acute stages of TMJPD treatment aims are to reduce pain and inflammation. In more sub-acute stage’s treatment can be progressed. When combined with dental consultation where splints and other means can be used advanced Soft tissue therapy modalities can be applied to the reduce muscle pain or referral patterns from trigger points and promote elongation of restricted muscle and connective tissue. Additional treatment involves addressing neck, back and shoulder imbalances. (Y Gursoy et al 2020) states that manual soft tissue therapy contributed to decreasing pain and improving TMJ movement. Low grade Joint mobilisation can be applied to encourage movement and corrective exercises such gentle stretching of tight TMJ, neck and shoulder muscles. Assisted and resisted movement exercises of the tmj muscles improve stability and coordination, additionally weaker neck and shoulder muscles are strengthened to improve a forward head position, (N S Mulla et al 2015)

( Simons & Travell, 1999)
( Simons & Travell, 1999)
states the combined use of low to moderate TMJ mobilisations and specific exercise performed over a two-week trial contributed to increased mouth range of movement. Patient education on ways to prevent excessive grinding, one sided dominance when chewing, altering foods while in acute episodes to limit aggravation, providing the patient with relaxation methods such as diaphragmatic breathing practice to reduce overuse of extra inspiratory muscles and reduce tension. The use of guided self-massage as instructed by the practitioner is also beneficial, moist heat or cold packs may be used on tight neck and shoulder muscles to reduce soreness. sleeping position can be addressed for e.g. if sleeping on one side predominantly or with the head and neck in poor alignment (Klasser & Epstein 2014).
A Multidisciplinary approach is considered the most effective approach to managing TMJPD as there can be many different contributing physical and psychological factors associated with TMJPD.
References
- Gursoy Y, Uysal H H, Osmanggazi E, 2020, Effects of manual therapy on range of motion, pain and quality of life in temporomandibular joint dysfunction. Journal of Romanian Sports Medicine Society (16,1)
- Klasser, Epstein, 2014, How to manage “closed lock” disc displacement without reduction with limited opening. JDCA
- Bonjardim L R, Gaviao M B D, Pereira L J, Castelo P M, 2005, Anxiety and depression in adolescents and the relationship between temporomandibular joint disorders. Quintessence Publishing Co, Vol 18,
- Prater S, 2012, TMJ and Massage Therapy: Structural Integration relieves muscle strain and tension: RDH Magazine
- Mulet M, decker K L, Look J O, Lenton P A, Schiffman E L, 2007 A randomised Clinical Trail assessing the efficacy of adding 6×6 exercises to self-care for the treatment of masticatory myofascial pain. Journal of Orofacial Pain.
- Mulla N S, Babu K V, Kumar N S, Rais R S, 2015 Effectiveness of Rocabado’s Technique for Subjects with Temporomandibular Joint Dysfunction, A single Blind Study. Int Jour Physiother. 2(1)
- Pundkar S, Patil D, Naqvi W, 2019, Effectiveness of Rocabado approach and Conventional Physiotherapy on pain, ROM and QOL in patients with TMJ Dysfunction: Comparative Study. Journal of critical reviews, vol. 6 (6)
- Al-Baghdadi M, Durhan J, Araujo-Soares V, Robalino S, Errinton L, Steel J, 2014 TMJ Disc Displacement without reduction management: A Systemic review. JDR Clinical Research Supplement, Vol. 93, (7), 2014.
- Toledo Jr E G D, Silva D P, Toledo J A D, Salgado I O, 2012 The Interrelationship between Dentistry and Physiotherapy in the treatment of Temporomandibular Disorders. TJCDP, Vol.13, (5)
- Westesson P L, Brooks S L, 1992 Temoromandiubuar Joint: Relationship between MR Evidence of Effusion and the Presence of Pain and Disk Displacement. AJR 159 (559-563).
- Bordoni B, Varacallo M. 2021, Anatomy Head and Neck, Temporomandibular Joint NCBI:
- Magee D J, 2008 Orthopaedic Physical Assessment Saunders 5th edition, St Louise Missouri
- Simons D G, Travell J G, 1999, Myofascial Pain and Dysfunction The Trigger Point Manual Vol 1. Williams & Wilkins, Maryland.
- Klasser G D, 2020, Internal Temporomandibular Joint Derangement. MSD Manual.
- arthritisaustralia.com.au/types-of-arthritis/fibromyalgia/
- www.cdc.gov/me-cfs/index.html




